Humanity has been recording the struggle against cancer since the disease was first described in ancient Egypt around 5000 years ago. The disease now claims some 10 million lives worldwide each year, and the World Health Organization predicts we will see more than 35 million new cancer cases by 2050.
“Technology is not a silver bullet to end cancer but it’s an enabler of the real heroes,” says Dr. Rowland Illing, Chief Medical Officer and Director of Global Healthcare and Nonprofits at AWS. “I’ve experienced first-hand how technology can make research more efficient and effective, diagnosis faster and more accurate, speed drug discovery and development, and increase accessibility through remote care and more inclusive clinical trials.”
Mapping the cancer landscape through genome sequencing
The Cancer Genome Atlas has collected data from nearly 20,000 tumours and comparative normal tissue samples from 11,328 patients across 33 cancer types. The visualisations produced through this data illustrate how different cancers develop and spread, including patterns in the cells where they originate, the role of different virus variants in triggering mutations, and the signalling pathways within the body that can be leveraged for effective treatments. The Atlas is part of the AWS Registry of Open Data, allowing researchers from around the world to expand their knowledge base.
Scaling this data-led approach to decoding cancer depends on sequencing the DNA of each potential patient cost-effectively. This is the goal of California-based Ultima Genomics. Ultima has developed a high-throughput, cost-effective next generation sequencer on AWS that can sequence an entire human genome, which cost $1,000 a decade ago, now for as little as $100.
Speeding up and democratising diagnosis
Genome sequencing of the type pioneered by Ultima Genomics can dramatically accelerate the detection of cancer through cost-effective genetic analysis. Munich Leukaemia Lab, which uses Amazon Elastic Compute Cloud (Amazon EC2) to accelerate its genomics data processing, has cut the compute time required from 20 hours to three, and improved both diagnostic speed and accuracy.
However, most patients won’t discover their cancer diagnosis through an in-depth genetic analysis. Many are simply visiting their doctor for a regular check-up, or perhaps a seemingly unrelated ailment. Identifying subtle visual indicators of the disease, even when it’s not the focus of the medical appointment, is one of the most important ways in which artificial intelligence (AI) is improving cancer survival rates.
“Cancer diagnosis still mostly works by pathologists looking down microscopes at tissue on glass slides,” says Michael Rivers, VP Digital Pathology at Roche Tissue Diagnostics, which has collaborated with Ibex and AWS to bring AI diagnostics tools to pathology labs through its Navify platform. “Digitising those slides gives us the potential to apply AI-based image analysis to help make a diagnosis and inform the treatment plan for a patient.”
As Rivers explains, one of the most dramatic ways in which AI can accelerate diagnosis involves training Foundational Models (FMs), within careful guidelines, to develop their own approach to analysing images. “Explainable AI is a really important component in the solutions we’re developing,” he says. “We provide heat maps and overlays to indicate to the pathologist how the algorithm is interpreting an image, but the pathologist has ultimate control over the final diagnosis.”
While breast cancer is a concern worldwide, diagnosing it in certain populations can present unique challenges. For example, Asian women typically have a relatively high density of breast tissue than other demographics which has historically made early detection more difficult.
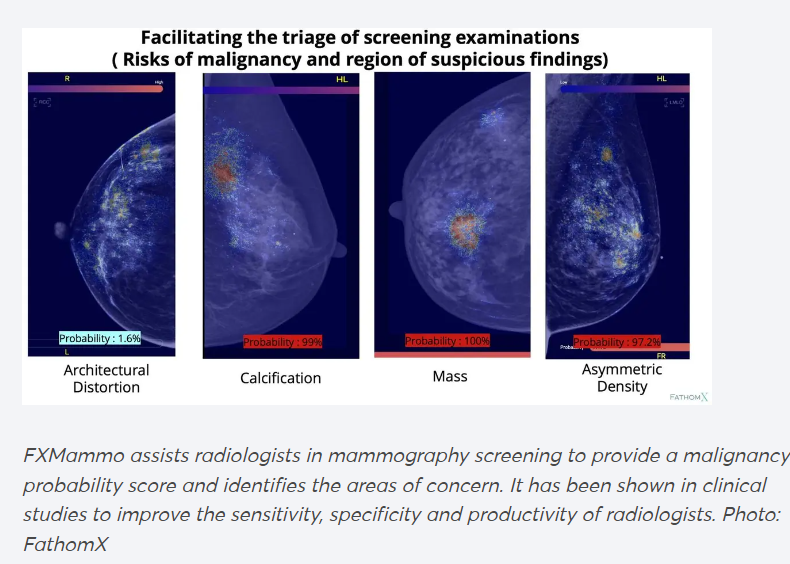
FathomX, a Singapore-based AI company originating from the National University of Singapore, has developed the FxMammo algorithm that addresses this issue. Using AI technology, FxMammo is designed to improve accuracy in identifying masses and abnormalities in dense breast tissue, offering more reliable and cost-effective early detection and reducing false positives by up to 75.5%.

Inclusive, personalised cancer treatment at scale
When healthcare providers are able to bring DNA-level insights about a patient’s cancer together with options for more personalised treatment, it can translate into better patient outcomes on a national scale. Genomics England sequences the DNA of cancer patients and their tumours in order to inform treatment. This includes highlighting the genes helping to spread cancer, the treatments most likely to affect them, and the likely side effects for each patient. A study supported by Genomics England data found that treatment for nine out of 10 brain tumours and bowel and lung cancers could be guided by genetic insights. Personalised treatments for cancer patients can involve targeted therapy drugs, a form of chemotherapy that zeroes in on the changes that make cancer cells different, and avoids some of the health impacts that come from blunter approaches killing healthy cells. Genomics England is building on this work using Anthropic’s Claude models on Amazon Bedrock to help researchers identify associations between genetic variants and medical conditions, including cancer.
Empowering cancer patients and carers everywhere
In remote regions of China, the limited availability of expert ultrasound operators is one of the most significant barriers to diagnosis. Shangyiyun has developed a breast cancer screening AI assistant, entitled Dr. J, to help fill this gap. Dr. J is able to detect and label lesions automatically, and upload ultrasound video and images to the cloud for additional, expert analysis. This is helping to scale the reach of breast cancer screening, and quickly identify cases in need of scrutiny. With AWS’s compute, storage, Dr. J can provide stable, efficient, and accurate screening services for institutions and users. AWS also provided a solid data security foundation for the global deployment of Dr. J.
Hurone AI uses predictive AI and Large Language Models (LLMs) built on AWS to help bridge gaps in cancer care in sub-Saharan Africa. It has built a two-way messaging system on AWS, which enables overstretched oncologists to monitor and support cancer patients at scale, even when local infrastructure is lacking. It’s exploring leveraging this same model to identify potential candidates for inclusion in clinical trials, which can play a vital role in developing treatment for all.
The complexity of the challenge that cancer presents to medicine is that each case, like the genes in each tumour, is unique. By making the campaign against cancer more individualiSed and more inclusive, and working alongside the more traditional methods and approaches, the cloud is helping turn this challenge into a strength. At the same time as enabling more personalised, targeted and effective treatment, it’s also delivering important psychological benefits. Helping each patient feel understood and supported on their own terms doesn’t just enable more targeted treatment; it contributes significantly to both patient experiences and patient outcomes.












